By Wylie Butler, Capstone Healthcare analyst
In 2021, the life expectancy at birth in the US decreased for the second consecutive year due largely to the COVID-19 pandemic and the opioid crisis. Despite per capita healthcare spending roughly twice that of other comparable countries, life expectancy in the US has not kept pace and has declined more significantly in recent years. Numerous bills, regulatory changes, and value-based care models have been introduced to address this issue but have largely fallen short in creating structural change. The Centers for Medicare and Medicaid Services (CMS) generally structure their value-based care models to accomplish three goals,
- Improve patient care, typically with an outcomes-based measure.
- Lower costs.
- Better align payment systems to promote patient-centered practices.
Over its first decade, five of the agencies’ 30 models produced net savings with mixed results on patient quality of care. One ongoing model is exploring the impact on quality of care for hospice to be carved into the Medicare Advantage benefit. Hospice care will never fit squarely into CMS’s box of quality-of-care measures. Clear wins are available – ensuring patients are treated with respect and efficient pain management, but outcome-based measures or focuses on improvements in patient health can’t apply. Death, and the final months leading up to it, remain an issue in healthcare that we typically approach by avoiding at all costs. The US needs a better model for hospice care that considers social determinants of health and refocuses the purpose of medicine in our final months.
The US needs a better model for hospice care that considers social determinants of health and refocuses the purpose of medicine in our final months.
Exhibit 1: US Life Expectancy and Spending per Capita Relative to Comparable Countries
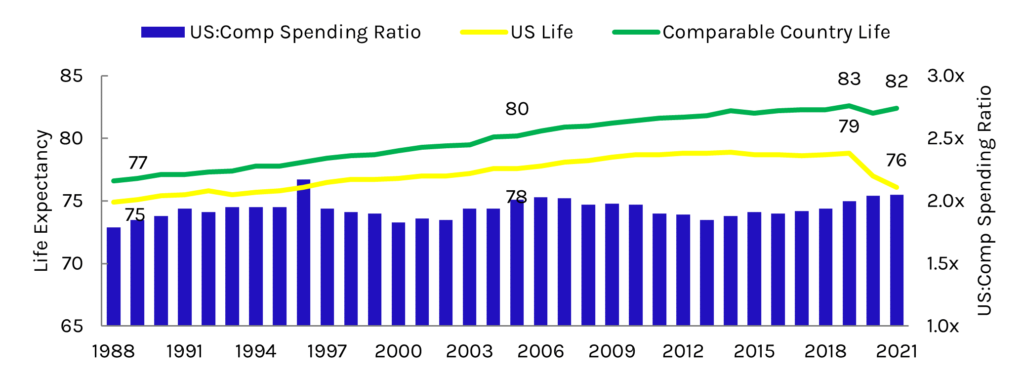
Source: Peterson-KFF Health System Tracker
End-of-life care is a relatively young part of the US healthcare system. Hospice care, which provides specialized palliative care for the dying, first took shape in the US during the 1960s despite being around in some form since the 11th century. Congress introduced the hospice benefit to Medicare in 1983, shortly after Jimmy Carter’s presidency, and who began his own hospice treatment this year. Use of the benefit has accelerated in recent years in line with overall growth in the Medicare population and the aging of our population.
While the basic quality of care measures remain important to control fraud, waste, and abuse in the industry, there is a common theme among Congressional hearings, MedPAC meetings, and CMS publications on the industry. Hospice discussions focus on the first two parts of CMS’s goals: costs and quality – spending cuts to reduce aggregate caps or new quality of care measures for providers to submit to CMS. Per MedPAC, access to care is estimated based on “trends in the supply of providers, utilization of hospice services, and Medicare marginal profit” and is seen as able to withstand pressure from regulators. However, a key failure slips through the cracks by limiting healthcare system evaluations to these measures. We focus entirely on the experience of patients in hospice, ignoring all those who are not receiving care.
The percentage of decedents in Medicare who used hospice has remained relatively stable over the last decade, while the use of hospice care is significantly lower in minority populations, men, and younger Medicare beneficiaries. This discrepancy in utilization by patient type raises further questions for policy advocates: what structural barriers limit access to care for minorities, and how can we remove them? What characteristics of the male population steer them away from hospice care? And in cases when death is not sudden, how can we better guide the younger Medicare population to the best choice for them in end-of-life care, whether in hospice or not?
Exhibit 2: Percent of Medicare Decedents Using Hospice
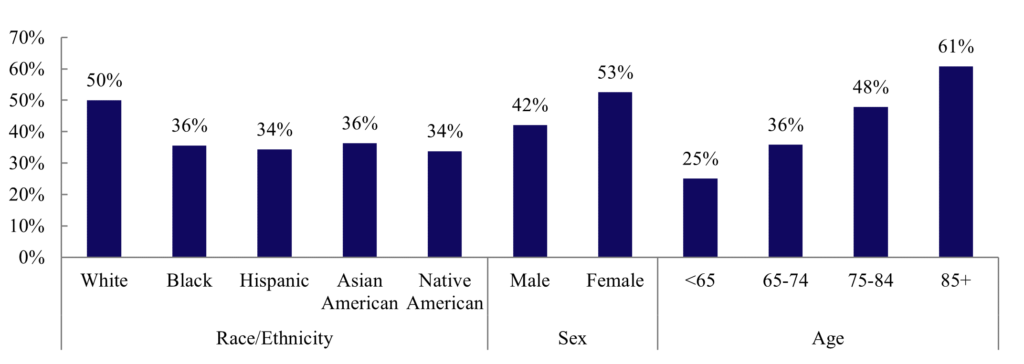
Source: MedPAC 2023 Report to Congress: Hospice
Elisabeth Kubler-Ross (On Death & Dying) and Atul Gawande (Being Mortal, which inspired me to my own career in healthcare policy) have both emphasized the need for reform in end-of-life care in the US Expansion in access to care must come from both sides of the physician-patient relationship. Physicians need to be better educated and prepared for end-of-life conversations, which should be a more prominent part of the medical school curriculum across specialties. As modern medicine pushes against biological limitations to extend life expectancy, physicians must increasingly recognize when care treatment should shift from focusing on curing illnesses and extending life to improving the quality of life for patients, even if it means a nearer death. Patients and their families also need to be better prepared for initiating and responding to these conversations and asking the questions that will guide them to a more meaningful life. All patients have a right to autonomy and a good life to the very end. The percentage of decedents using hospice will not ever be 100%, but the current system and inconsistencies in utilization within suggest significant work remains.
The percentage of decedents using hospice will not ever be 100%, but the current system and inconsistencies in utilization within suggest significant work remains.
Capstone will continue to follow and untangle future value-based care efforts within the hospice world and their impacts on post-acute care in the US as the ways our population lives and dies continue to evolve. We expect opportunities in value-based care to continue to evolve in CMMI’s second decade and that the role of both providers and patients will change significantly.

Wylie Butler, Capstone Healthcare analyst
Read more from Wylie:
The Edge of the Cliff: Why the Potential Fiscal Crisis Will Drive Healthcare Policy
Read Wylie’s bio here.